Home

 The Canadian Association of Nurses in HIV/AIDS Care (CANAC) is a national professional nursing organization committed to fostering excellence in HIV/AIDS nursing, promoting the health, rights and dignity of persons affected by HIV/AIDS and to preventing the spread of HIV infection.
The Canadian Association of Nurses in HIV/AIDS Care (CANAC) is a national professional nursing organization committed to fostering excellence in HIV/AIDS nursing, promoting the health, rights and dignity of persons affected by HIV/AIDS and to preventing the spread of HIV infection.
CANAC’s members hail from all regions of Canada working in clinical practice, education, research and/or administration. We have a proud history of working in collaboration with other nursing organizations and with the international HIV/AIDS community. Volunteerism and solidarity with those affected by HIV/AIDS are the heart and soul of our organization.

What’s New
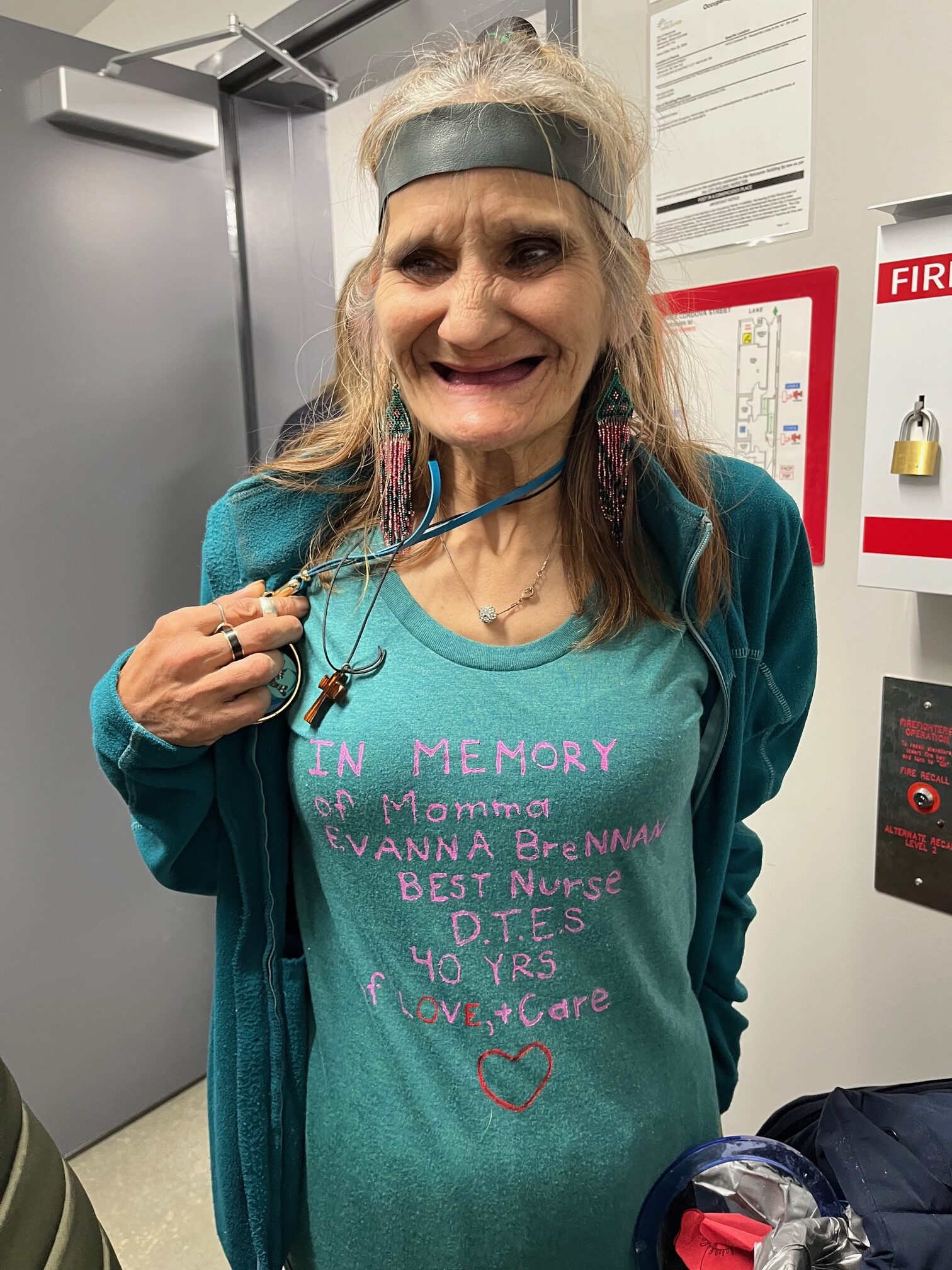
Honouring a Canadian leader in HIV/AIDS Care – Evanna Brennan
January, 2025
Evanna Brennan was a longtime CANAC member and leader in HIV/AIDS care with her trailblazing work in Vancouver’s Downtown Eastside.
CANAC has shared Evanna’s work in the past – showcasing her, and collaborator Susan Giles in the showing and panel discussion of the film Angels on Call in February 23, 2023.
Evanna sadly passed in October 2023, but just this past December, Lookout Housing and Health Society opened a supportive housing project for older adults with medical needs in Vancouver’s Downtown Eastside (DTES). The new building was named after Evanna Brennan. The opening of the Brennan Building was a wonderful event this past week and helped celebrate the amazing work of Evanna. Here is what Lookout Housing and Health Society said about Evanna and Susan Giles:
“Susan and Evanna were the dynamic duo, working in the downtown eastside to provide care to the community’s most vulnerable individuals while pioneering harm reduction for patients in their care. They insisted on bringing healthcare to where it was needed most – in the shelters and single room occupancy hotels where their patients lived.”
CANAC is honoured to have shared Evanna’s contribution to street nursing and HIV care. We have provided photos from the opening of the supportive housing project named in her honour and links to the Angels on Call film below.
-

- Event attendees and CANAC members attending the event: (from left to right) Dr. Vera Caine, Susan GIles, Dr. Jane McCall and Irene Goldstone
Angels on Call
Street nurses Evanna Brennan, 75, and Susan Giles, 68, have foregone retirement to provide full-time care to the desperately ill, homeless, alcoholic and drug-addicted residents of Vancouver’s poverty-stricken Downtown Eastside. Directed and produced by Roberta Staley. Co-directed and co-produced by Tallulah. Funded by Telus StoryHive.
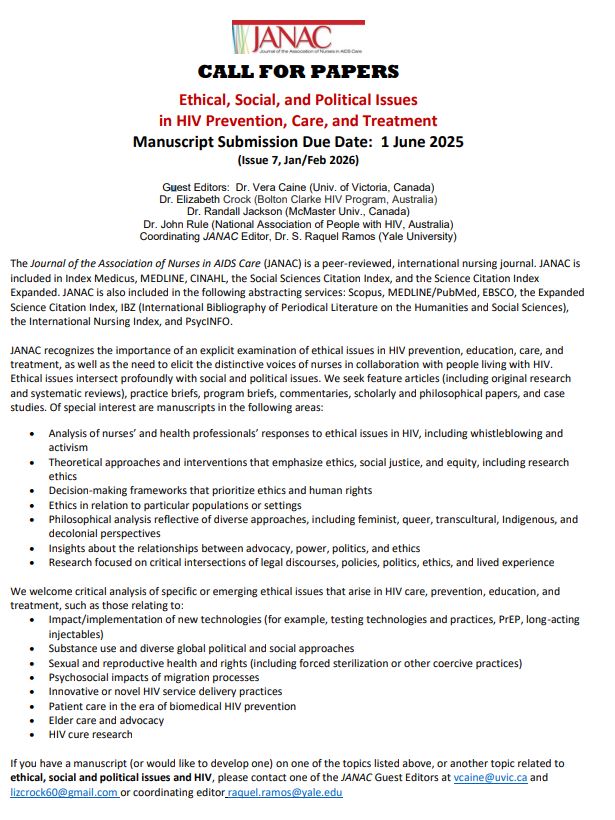
JANAC Call for Papers
January, 2025
CANAC is excited to share the call for a special JANAC issue.
The attached call for papers on Ethical, Social and Political Issues in HIV Prevention, Care and Treatment may align with many of the ongoing advocacy, care, and research of our members!
Please review the attached document for more information.
This is also a great reminder that all CANAC members have access to the Journal of the Association of Nurses in HIV/AIDS Care. If you have any issues accessing the journal, please reach out to info@canac.org
A conversation between Dr. Theresa Tam and Jade Elektra
March, 2024
CANAC is excited to share an interview led by a Public Health Agency of Canada (PHAC) team, including Sophia Neumann and Jessica Helwig, on their awareness campaign on the Undectectable=Untransmisible (U=U) initiative.
A conversation between Dr. Theresa Tam and Jade Elektra
Undetectable = Untransmittable (U=U) refers to the scientific consensus that HIV cannot be sexually transmitted when a person living with HIV consistently takes antiretroviral therapy (ART) and the amount of HIV in their blood remains very low—so low that it cannot be detected by many standard HIV tests.
While the U=U message empowers people living with HIV and reduces stigma associated with the virus, it is only effective if individuals living with HIV are able to continuously take their medication. Many people in Canada, such as African, Caribbean and Black communities, Indigenous Peoples, gay, bisexual, and other men who have sex with men, people who use drugs, and incarcerated people, face social and structural barriers that can impact access to HIV care and make it difficult to maintain consistent access to treatment. In order for U=U to have the greatest impact, people living with HIV must be supported by promoting U=U, advocating for those who face barriers in medication adherence, and facilitating access to care. All public health and health professionals can help normalize and share the U=U message.
Dr. Theresa Tam, Canada’s Chief Public Health Officer, had a discussion with Jade Elektra, HIV Activist, drag performer, recording artist, and community builder about the social and structural nuances of U=U.
Dr. Theresa Tam: Jade, it’s a pleasure speaking with you about U=U. You’ve done so much to create safe spaces and address HIV-related stigma. The magazine you’ve founded by and for people living with HIV is just one example. I’m looking forward to delving into this topic with you.
Jade Elektra: Thank you, Dr. Tam. I’m always happy to talk about U=U—it’s a topic close to my heart and one that needs more attention.
Jade Elektra: U=U can have a tremendous impact on a person living with HIV, especially if they are sexually active, and can be empowering for young people and recently diagnosed folks living with HIV. However, I’d be interested in hearing your perspective as a public health leader on why U=U is so important.
Dr. Theresa Tam: Looking back, it’s amazing to see how far treatment and care for HIV has come in the past 45 years. Thanks to scientific advances, HIV has become a treatable chronic condition. Don’t get me wrong, we still have a ways to go, but now people with HIV are living longer and healthier lives than before. People living with HIV who are aware of U=U are more likely to report better mental, physical and sexual health. This science has transformed what it means to live and love with HIV on a global scale.
However, we also need to address the stigma and discrimination experienced by people living with HIV, both socially and within healthcare settings. It can really affect people’s wellbeing, including their willingness to seek out testing and treatment.
Jade Elektra: Yes, there are many barriers that could contribute to not achieving an undetectable status.
Dr. Theresa Tam: In 2020, close to 17,000 people in Canada did not achieve viral suppression. Because they lacked access to effective HIV treatment options or didn’t take any treatments, they were still at risk of transmitting HIV. The U=U message is important because it reduces HIV-associated stigma and encourages people to access testing and treatment needed to reach an undetectable status. As much as there is still work to be done, Canada has made great strides and has already reached one of the UNAIDS interim HIV treatment targets for the year 2025 of ensuring 95% of people with HIV who are on treatment have a suppressed viral load.
Dr. Theresa Tam: We know that there are barriers to becoming undetectable. Jade, could you share your views on what might prevent someone from achieving “undetectable” status?
Jade Elektra: Yes there are many possible contributing barriers such as, lack of education, racism, and limited access to healthcare facilities. African, Caribbean, and Black communities in particular experience higher rates of HIV, but these communities may also face more systemic and structural barriers preventing access to medication. Some people may have to choose between buying food, paying rent or getting their medication. Other folks may experience: intermittent access to treatment; multiple health problems at once; or precarious housing without a set routine. Any of these situations affects their ability to stick to a treatment plan. What’s more, people may be reluctant to continue seeking care if they experience racism in health care settings or cannot access culturally appropriate care. But I believe the stigma of being HIV+, or even being perceived as being HIV+, is the biggest hurdle.
Dr. Theresa Tam: Clearly there are complex and compounding systemic factors that may impact someone’s ability to consistently take medication or access testing and care to begin with.
Jade Elektra: Definitely – I went many years without any medical treatment and was extremely ashamed and felt afraid to let anyone know that I was HIV+. I believe that shame and fear actually made my health worse. But once I started the retro-viral meds and started watching my numbers get better I took pride in taking care of myself.
That said, not everyone who is living with HIV has access to medical treatment or an adherence routine due to the factors we’ve been talking about. The shame and fear these individuals may feel might be reinforced by general HIV-related stigma, not being able to reach viral suppression, or even specific health care related stigma. They may face discrimination and judgement by health professionals for not adhering to treatment or not getting support in leading full social and sexual lives. They may even be labelled as “non-compliant” in adhering to medication, which adds to the stigma, when in fact the barriers these individuals face are systemic and not a reflection of a personal failing.
Dr. Theresa Tam: For patients who face barriers to U=U, it is important for us, as health professionals, to recognize our own personal biases and avoid stigmatizing patients that aren’t adhering to medication. As health professionals, it is important we take a person-centered approach and provide support that meet patients’ needs.
Jade Elektra: I feel strongly that health professionals need to support patients living with HIV, especially those who face barriers to U=U. U=U should be a practiced, normalized conversation with patients and clients, and awareness of barriers should be well known. I have experienced healthcare settings where the provider is not promoting U=U or doesn’t know about it. What would you recommend health professionals do to support patients with HIV who face barriers to U=U?
Dr. Theresa Tam: Not just as health professionals, we need to normalize sexual health and sexual health conversations, including sexually transmitted and blood-borne infections to reduce stigma associated with HIV testing and treatment.
We can continue to support patients who face barriers to U=U by promoting the full range of effective, evidence-based prevention options for HIV and other sexually transmitted and blood-borne infections, like condoms, pre-exposure prophylaxis (PrEP), post-exposure prophylaxis (PEP), and harm reduction. We can connect patients with other health or social services, which may then help address the barriers our patients face to reaching undetectable. How do we encourage health professionals to champion U=U while also meeting patients where they are at?
Jade Elektra: I believe a bigger push to educate all health professionals, people living with HIV, and the general public at large about U=U could help close the gap. Pamphlets in waiting rooms and clinics and displaying posters in public areas is a great way to start the conversation. Now we can add the Public Health Agency of Canada’s recent public awareness campaign on U=U and its helpful resources such as the Communication Tips for Health Professionals factsheet. Another good source of information is CATIE—a community-based organization promoting good practices for prevention and treatment and they also have great HIV and U=U related materials available, free of charge. We need the information widely available in the public sphere.
Encouraging patients to ask questions is another great way to start the conversation and meet people where they are at. Health professionals can ask patients about their situation and the barriers they may face to learn how to best support their health needs. Always remember that each person has their own circumstances of why they can or cannot achieve a U=U status. It’s helpful to focus on what can be done to support patients within their unique circumstances.
Dr. Theresa Tam: Thank you, Jade, for taking the time to speak about U=U and openly sharing your thoughts and experiences. Our conversation today emphasizes that all health professionals, whether or not they work in sexual health or HIV specific fields, have the power to create positive change through initiating and promoting conversations about HIV, U=U, and safer sex. To learn more about U=U and to access resources for health professionals, please visit Canada.ca/HIV
Une conversation entre la Dre Theresa Tam et Jade Elektra
L’expression « indétectable = intransmissible » (I = I) fait référence au consensus scientifique selon lequel le VIH ne peut pas être transmis sexuellement lorsqu’une personne vivant avec celui-ci suit systématiquement un traitement antirétroviral (TAR) et que la quantité de VIH dans son sang demeure très faible – si faible qu’elle ne peut pas être détectée par de nombreux tests standard de dépistage.
Si le message I = I habilite les personnes vivant avec le VIH et réduit la stigmatisation associée au virus, il n’est efficace que si les personnes vivant avec le VIH sont en mesure de prendre leurs médicaments de manière continue. De nombreuses personnes au Canada, telles que les communautés africaines, caribéennes et noires, les peuples autochtones, les homosexuels, les bisexuels et les autres hommes ayant des rapports sexuels avec des hommes, les consommateurs de drogues et les personnes incarcérées, sont confrontées à des obstacles sociaux et structurels qui peuvent avoir une incidence sur l’accès aux soins liés au VIH et rendre difficile le maintien d’un accès cohérent au traitement. Pour que le programme I = I ait le plus grand impact possible, il faut soutenir les personnes vivant avec le VIH en promouvant le programme I = I, en défendant les personnes confrontées à des obstacles en matière d’observance thérapeutique et en facilitant l’accès aux soins. Tous les professionnels de la santé publique et de la santé peuvent contribuer à normaliser et à partager le message de l’accès universel.
La Dre Theresa Tam, administratrice en chef de la santé publique au Canada, a discuté avec Jade Elektra, militante de la lutte contre le VIH, artiste de drag et de studio et bâtisseuse de communauté, des nuances sociales et structurelles de I = I.
Dre Theresa Tam : Jade, c’est un plaisir de vous parler de I = I. Vous avez tant fait pour créer des espaces sûrs et lutter contre la stigmatisation liée au VIH. Le magazine que vous avez fondé par et pour les personnes vivant avec le VIH n’en est qu’un exemple. J’ai hâte d’approfondir ce sujet avec vous.
Jade Elektra : Merci, Dre Tam. Je suis toujours heureuse de parler de I = I – c’est un sujet qui me tient à cœur et qui a besoin de plus d’attention.
Jade Elektra : I = I peut avoir un impact considérable sur une personne vivant avec le VIH, en particulier si elle est sexuellement active, et peut donner du pouvoir aux jeunes et aux personnes récemment diagnostiquées comme vivant avec le VIH. Cependant, j’aimerais connaître votre point de vue en tant que responsable de la santé publique sur les raisons pour lesquelles I = I est si important.
Dre Theresa Tam : Avec le recul, il est étonnant de voir à quel point le traitement et la prise en charge du VIH ont progressé au cours des 45 dernières années. Grâce aux progrès scientifiques, le VIH est devenu une maladie chronique traitable. Ne vous méprenez pas, il reste encore du chemin à parcourir, mais aujourd’hui, les personnes séropositives vivent plus longtemps et en meilleure santé qu’auparavant. Les personnes vivant avec le VIH qui connaissent I = I sont plus susceptibles de faire état d’une meilleure santé mentale, physique et sexuelle. Cette science a transformé ce que signifie vivre et aimer avec le VIH à l’échelle mondiale.
Toutefois, nous devons également nous attaquer à la stigmatisation et à la discrimination dont sont victimes les personnes vivant avec le VIH, tant sur le plan social que dans les établissements de soins de santé. Cela peut réellement affecter le bien-être des personnes, y compris leur volonté de se faire dépister et traiter.
Jade Elektra : Oui, il existe de nombreux obstacles qui peuvent nuire à l’atteinte du statut indétectable.
Dre Theresa Tam : En 2020, près de 17 000 personnes au Canada n’ont pas atteint la suppression virale. Parce qu’elles n’ont pas eu accès à des traitements efficaces contre le VIH ou qu’elles n’ont pris aucun traitement, elles risquent toujours de transmettre le VIH. Le message I = I est important parce qu’il réduit la stigmatisation associée au VIH et encourage les gens à accéder aux tests et aux traitements nécessaires pour atteindre un statut indétectable. Même s’il reste du travail à faire, le Canada a fait de grands progrès et a déjà atteint l’un des objectifs intermédiaires de l’ONUSIDA en matière de traitement du VIH pour l’année 2025, à savoir garantir que 95 % des personnes séropositives qui suivent un traitement ont une charge virale supprimée.
Dre Theresa Tam : Nous savons qu’il existe des obstacles pour devenir indétectable. Jade, pourriez-vous nous faire part de votre point de vue sur ce qui pourrait empêcher quelqu’un d’atteindre le statut « indétectable »?
Jade Elektra : Oui, il existe de nombreux obstacles possibles, tels que le manque d’éducation, le racisme et l’accès limité aux établissements de santé. Les communautés africaines, caribéennes et noires en particulier connaissent des taux de VIH plus élevés, mais ces communautés peuvent également être confrontées à des obstacles plus systémiques et structurels empêchant l’accès aux médicaments. Certaines personnes doivent parfois choisir entre acheter de la nourriture, payer leur loyer ou obtenir leurs médicaments. D’autres personnes peuvent être confrontées à un accès intermittent au traitement, à des problèmes de santé multiples à la fois ou à un logement précaire sans routine fixe. Chacune de ces situations affecte leur capacité à suivre un plan de traitement. De plus, les personnes peuvent hésiter à continuer à se faire soigner si elles sont victimes de racisme dans les établissements de soins ou si elles n’ont pas accès à des soins adaptés à leur culture. Mais je pense que la stigmatisation liée au fait d’être séropositif, ou même d’être perçu comme tel, est le plus grand obstacle.
Dre Theresa Tam : Il est clair qu’il existe des facteurs systémiques complexes et cumulés qui peuvent avoir un impact sur la capacité d’une personne à prendre régulièrement ses médicaments ou à accéder aux tests et aux soins.
Jade Elektra : Absolument. J’ai passé de nombreuses années sans aucun traitement médical, j’avais extrêmement honte et j’avais peur de dire à qui que ce soit que j’étais séropositive. Je crois que cette honte et cette peur ont en fait aggravé mon état de santé. Mais une fois que j’ai commencé à prendre des médicaments antiviraux et que j’ai commencé à voir mes chiffres s’améliorer, j’ai été fière de prendre soin de moi.
Cela dit, toutes les personnes vivant avec le VIH n’ont pas accès à un traitement médical ou à une routine d’observance en raison des facteurs dont nous avons parlé. La honte et la peur que ces personnes peuvent ressentir peuvent être renforcées par la stigmatisation générale liée au VIH, l’incapacité à atteindre la suppression virale ou même la stigmatisation spécifique liée aux soins de santé. Elles peuvent être confrontées à la discrimination et au jugement des professionnels de la santé parce qu’elles ne suivent pas leur traitement ou ne sont pas aidées à mener une vie sociale et sexuelle épanouie. Elles peuvent même être qualifiées de « non-conformistes » dans l’observance de leur traitement, ce qui ajoute à la stigmatisation, alors que les obstacles auxquels ces personnes sont confrontées sont systémiques et ne sont pas le reflet d’une défaillance personnelle.
Dre Theresa Tam : Pour les patients qui se heurtent à des obstacles à I = I, il est important que nous, en tant que professionnels de la santé, reconnaissions nos propres préjugés et évitions de stigmatiser les patients qui ne respectent pas leur traitement. En tant que professionnels de la santé, il est important d’adopter une approche centrée sur la personne et de fournir un soutien qui réponde aux besoins des patients.
Jade Elektra : Je suis convaincue que les professionnels de la santé doivent soutenir les patients vivant avec le VIH, en particulier ceux qui se heurtent à des obstacles à l’accès à l’information. L’accès à l’information devrait être une pratique courante, une conversation normalisée avec les patients et les clients, et la connaissance des obstacles devrait être bien connue. J’ai connu des établissements de santé où le prestataire n’encourageait pas l’accès à l’information ou n’était pas au courant de son existence. Que recommanderiez-vous aux professionnels de la santé de faire pour aider les patients séropositifs qui se heurtent à des obstacles à l’accès à l’information?
Dre Theresa Tam : Pas seulement en tant que professionnels de la santé, nous devons normaliser la santé sexuelle et les conversations sur la santé sexuelle, y compris les infections sexuellement transmissibles et les infections transmises par le sang, afin de réduire la stigmatisation associée au dépistage et au traitement du VIH.
Nous pouvons continuer à soutenir les patients qui se heurtent à des obstacles à I = I en promouvant l’ensemble des options de prévention efficaces et fondées sur des données probantes pour le VIH et d’autres infections sexuellement transmissibles et transmissibles par le sang, comme les préservatifs, la prophylaxie pré-exposition (PrEP), la prophylaxie post-exposition (PPE) et la réduction des risques. Nous pouvons mettre les patients en contact avec d’autres services sociaux ou de santé, qui peuvent alors les aider à surmonter les obstacles auxquels ils se heurtent pour devenir indétectables. Comment encourager les professionnels de la santé à défendre l’approche I = I tout en rencontrant les patients là où ils en sont?
Jade Elektra : Je pense qu’un effort plus important pour éduquer tous les professionnels de la santé, les personnes vivant avec le VIH et le grand public au sujet de I = I pourrait aider à combler le fossé. Des brochures dans les salles d’attente et les cliniques et des affiches dans les lieux publics sont un excellent moyen d’entamer la conversation. Nous pouvons maintenant ajouter la récente campagne de sensibilisation de l’Agence de santé publique du Canada sur le thème de l’obligation d’uriner et ses ressources utiles telles que la fiche d’information sur les Conseils de communication pour les professionnels de la santé. Une autre bonne source d’information est CATIE, une organisation communautaire qui promeut les bonnes pratiques en matière de prévention et de traitement, et qui met gratuitement à disposition d’excellents documents sur le VIH et I = I. L’information doit être largement diffusée dans la sphère publique.
Encourager les patients à poser des questions est un autre excellent moyen d’entamer la conversation et de rencontrer les gens là où ils en sont. Les professionnels de la santé peuvent interroger les patients sur leur situation et les obstacles qu’ils peuvent rencontrer afin d’apprendre comment répondre au mieux à leurs besoins en matière de santé. N’oubliez jamais que chaque personne a ses propres circonstances qui expliquent pourquoi elle peut ou ne peut pas atteindre le statut I = I. Il est utile de se concentrer sur ce qui est le plus important pour elle. Il est utile de se concentrer sur ce qui peut être fait pour soutenir les patients dans leur situation particulière.
Dre Theresa Tam : Merci, Jade, d’avoir pris le temps de parler de I = I et d’avoir partagé ouvertement vos pensées et vos expériences. Notre conversation d’aujourd’hui souligne que tous les professionnels de la santé, qu’ils travaillent ou non dans le domaine de la santé sexuelle ou du VIH, ont le pouvoir de créer un changement positif en lançant et en promouvant des conversations sur le VIH, I = I et le sexe à moindre risque.
Pour en savoir plus sur I = I et accéder aux ressources destinées aux professionnels de la santé, veuillez consulter le site Canada.ca/VIH.
Call for Abstracts – CANAC Conference 2024
December, 2023
Call for Abstracts is now open until February 16, 2024!
Please send any questions or inquiries to canachq@gmail.com
World AIDS Day 2021 – Remember. Reflect. Renew.
November, 2021
On this World AIDS Day, I ask you to take time to remember, reflect, and renew your commitment to the important work you do as a nurse or healthcare provider. Each year World AIDS Day gives us an opportunity to remember those we have lost to HIV disease and other pandemics. It also allows us to remember why we do the work we do. This day gives us an opportunity to reflect on the lives we have changed and will change as well as how we can continue engage in self-care that allows us to do the work we do. World AIDS Day also gives us an opportunity to renew our commitment to ourselves and those we serve. This period of renewal aligns with the approach of the winter season which in many Indigenous cultures is a time for renewal and rejuvenation. It is the season when much of Canada and the northern hemisphere enter the slumber that renews life that manifests prominently during spring. This year we are at an inflection point with the SARS CoV-2 (COVID-19) pandemic when we are seeing progress while navigating hurdles that continue to lay bare social and political upheavals, we must navigate to weather the transition from a pandemic to an endemic state where we live with SARS CoV-2. As we move forward, it is important for us to heed the concern expressed in the UNAIDS theme for World AIDS Day 2021, “End inequalities. End AIDS. End pandemics.” As we strive to achieve these goals, remembering, reflecting, and renewing our commitments will help us achieve the goals espoused in this theme that are grounded in human rights-based approaches to caring for ourselves and our communities.
In humility and respect,
J. Craig Phillips, LLM, PhD, RN, ACRN, FAAN, FCAN
CANAC President
World AIDS Day 2020 – Global Solidarity, Shared Responsibility
December, 2020
The theme for the 2020 Worlds AIDS Day is Global Solidarity, Shared Responsibility. It is an important focus given that the need for global solidarity has never been greater. While significant advances in an effort to end HIV have been lost due to the impact of the COVID19 pandemic, particularly for women and girls, now is the time to imagine a different world. As we seek solidarity it is important that we challenge colonial systems and their power structure and to advocate for freedom and plurality, as foundational to solidarity. Over the past few months, we have seen that the actions of politicians create greater inequities and reinforce differences both locally and globally. It is now that we must demand that we make different choices. Choices about how we want to live together, choices that will allow us to have a world that is marked by global solidarity and shared responsibilities. There is a great need to challenge, to raise questions, and to demand how we build a world in which we emphasize democracy, human rights, and equity. The call for shared responsibility demands that we engage in thinking that has ethical and political implications. This is the time that we need to call forth the knowledge we have gained in the context of the HIV movement. Solidary is a necessity and shared responsibility only one small step of addressing the impact HIV has had and continues to have on all of our lives.
This year, Giving Tuesday coincides with World AIDS Day! So, on Dec. 1, we are asking all our members and supporters to help organizations whose work focuses on HIV/AIDS. Together we do make a difference.
Warmly,
Vera Caine PhD, RN
CANAC President
ICN accepts IAS Presidential Award on behalf of the world’s nurses
July, 2020
We Stand in Solidarity
June, 2020
CANAC stands in solidarity with the Black Lives Matter movement and alongside activists across Canada, the US and globally. Racism resonates deeply across many communities we work with and causes profound harm. The institutional racism within healthcare and within the criminal justice system deeply impacts people living with HIV. The persistent disparities, caused by public policies and practices, are visible in access to health care, housing, education, income and employment.
As nurses working in HIV/AIDS care we promote social justice, culturally safe care and human rights. We strive towards this in our practices, education, and research. Alongside other organizations working with people living with HIV, we will challenge institutional racism, inequities, and human rights violations. We support our members and ally organizations in efforts to address white privilege and anti-Black racism.
At the same time, CANAC nurses recognize that the effects of and ongoing colonization in Canada have resulted in significant health disparities in Indigenous populations. This includes an increased risk of acquiring HIV and an increased likelihood of being victims of violence and racism. We are working to decolonize our practices and promote allyship. The systematic and daily racism needs to stop.
In solidarity,
CANAC
CANAC’s Position Statement on Undetectable = Untransmittable
June, 2020
In congruence with science and robust evidence CANAC endorses the ‘Undetectable equals Untransmittable’ (U=U) position. U=U affirms that people living with HIV who maintain an undetectable viral load cannot transmit HIV through sexual activities. For the entire position statement, click here.
Strategic Plan 2019 – 2023
June, 2020
CANAC 2020 Conference Postponed due to COVID-19
March, 2020
March 13th, 2020
The Canadian Association of Nurses in HIV/AIDS Care (CANAC/ACIIS) is postponing its annual conference due to the Novel Coronavirus 2019 (COVID-19). This unanimous decision was reached by the CANAC board and supported by our preconference partners the Harm Reduction Nurses Association (HRNA) and the Alberta Coalition of Nurses for Harm Reduction (ANCHR).
For over a year, we have anticipated that we would gather in 2020 to share practices and research that highlight the conference theme of Advocate. Inspire. Change. We value our annual face-to-face meetings – as they are rich and meaningful places of learning and places where we can network and celebrate each other’s work and accomplishments.
Sadly, the spread of the coronavirus makes it impossible to gather in May and it would be irresponsible of us to encourage attendance when those who come, could be exposed. Many health care workers, particularly nurses are also being called to assist in managing the pandemic.
Over the next twelve months, once COVID 19 no longer restricts all of our lives, we will plan to host local events across the country to ensure that members can come together to network and learn from each other. We received stellar, thought provoking and inspiring abstracts for workshops and presentations. We will work with those who submitted abstracts to share their work through our newsletters or through webinairs. We hope that the amazing keynote speakers, who enthusiastically had agreed to come to our conference will come next year.
One of CANAC’s most wonderful strengths has been its annual conference. Those who have already registered for the conference will receive full refunds of their registration fee. If you have booked hotels and flights, we encourage you to cancel these and any other arrangements, but we cannot control flight cancellation costs.
We are most grateful for your ongoing support, as the success of our annual meetings depends on all of you in creating a common sense of purpose. We look forward to seeing you in 2021 in Edmonton. Stay tuned, you will hear from us soon again.
– Members of the CANAC/ACIIS Board, the HRNA board, and the ANCHR board
CANAC Endorses HIV2020
February, 2020
World AIDS Day 2019
December, 2019
This year the theme for World AIDS Day is Communities Make the Difference. It is an important theme that recognizes the value of community and that much happens when people come together. Communities have come together to provide care, to tackle stigma and to create spaces where people are recognized and remembered. Some of these communities are being led by people living with HIV; other communities are being led by nurses in an effort to provide care, challenge discrimination and ensure human rights are being upheld.
There are many examples that show what can happen when communities come together. Here is one example, which is inspiring, shared by Jeff Rheinhart, the current treasurer of CANAC:
In July of 2018, I attended a planning meeting around gay men’s health in Toronto, hosted by the Ontario HIV Treatment Network (OHTN). While there, I found myself in a small breakout session with other healthcare providers, community workers and people living with HIV to discuss healthcare access for people with HIV who do not have immigration status or health insurance in Canada. There was a willingness in the room to respond to the needs of people who live in Canada ‘undocumented and uninsured’. One year later, in August 2019, we opened the Blue Door Clinic.
The Blue Door, at its heart, represents a combination and culmination of all of the important lessons we’ve learned about HIV care since the 80s. As a clinic specializing in HIV treatment and care for people who are precariously insured or who lack access to care due to immigration status or insurance status in Toronto, the clinic aims to make a dent in the remaining 10-10-10 of the cascade. Many in the HIV movement consider this part of the cascade where priority efforts are needed to curb the epidemic. But aside from those high level policy foci, I started to think more about the Clinic’s operation and its relationship to some of the ideals of HIV nursing.
We often think about GIPA and MIPA (greater and meaningful involvement of people with HIV/AIDS), but sometimes have a hard time translating that into practice. For Blue Door, part of GIPA/MIPA had to be listening to people with HIV for years, some of whom reported to us that, despite efforts to meet their needs, their immigration status still made it hard to access care; listening and holding that in our minds, waiting for the stars to align, like they did that day in July 2018, to make a move towards making a change. As nurses, we hear about the challenges of our clients, respond to what we can within the systemic limits around us and foster patience in ourselves to be able to change the system when opportunities arise.
From the beginning of the movement, community collaborating was a cornerstone of the HIV response. And so community and ASO partners are cornerstone to the Blue Door’s success, helping to identify people who could use the service and support them as they navigate through the medical pieces of HIV care. Clinically, we know that interdisciplinary care improves outcomes for clients. The Blue Door works with doctors, nurses, social workers, case managers, coordinators, peer workers, reception staff and managers to respond to client needs. This holistic care would not be possible without the combined partnership of ten different health and social service agencies.
All of this comes together for just 6 hours each month of clinic time. A tiny grain of sand in the hourglass that makes up all the time spend to address HIV and its impact. But a grain of sand that is impactful, meaningful and collaborative and one that I am proud to share with you on World AIDS day.
We hope you will find time this week to join your local communities in an efforts to address pressing issues in HIV care, treatment and prevention, and to draw attention to the importance of protecting the human rights of people living with HIV.
“Cook your Wash” Campaign
September, 2019
This year’s annual CANAC Conference welcomed Dr. Michael Silverman, Lawson Associate Scientist and Chair/Chief of Infectious Diseases at the Schulich School of Medicine & Dentistry, Western University, London Health Sciences Centre and St. Joseph’s Health Care London as a plenary speaker at the PreConference day. This day highlighted work that is being done in London, ON to combat the declared HIV/HCV crisis. One of the ways the outbreak in London is being tackled is through the “Cook Your Wash” Campaign, research done by Dr. Silverman and other researchers at Lawson Health Research Institute and Western University.
The Ontario Harm Reduction Distribution Program (OHRDP) and The Ontario Harm Reduction Network (OHRN) have created a document that summarizes and emphasizes key messaging surrounding this campaign.
Be sure to check out this document and also the published studies in the Journal of Acquired Immune Deficiency Syndrome (JAIDS) – free without subscription. There will be prompting for a sign in, click cancel and go back on your browser.
https://www.catie.ca/sites/default/files/ohrdp-ohrn-note-findings-05032019.pdf
https://journals.lww.com/jaids/pages/results.aspx?txtKeywords=silverman+injection+drug
CANAC Nurses published in JANAC
April, 2018
Childhood Sexual Abuse in a Population of Patients Living With HIV: Prevalence and Impact by Jane McCall, MSN, RN, Patricia Lauridsen-Hoegh, BSN, LLB, RN, Dave Unger, BA, MSc, MD, CCFP, FCFP, J. Craig Phillips, LLM, PhD, RN, ARNP, ACRN, FAAN, Julie Kille, BSN, MSN, RN.
CANAC launches new Online Membership Portal
October, 2017
CANAC’s Online Member Portal will be a place for you to renew your membership, set your contact preferences, update your contact information, and allow us to send you timely communication and manage our conferences and events in, all in one place. This software is hosted by member365, who we have been working closely with to ensure the program meets our needs.
By now, members will have received a welcome email with a username and password for the new Online Member Portal. Make sure and renew your membership by November 1st to stay up-to-date with CANAC news and events.
Existing members can login to CANAC’s Online Membership Portal to maintain your membership.
If you have questions about the Portal, or did not receive your username, please contact us at ontariocanac@gmail.com.
Illicit drug overdoses in BC: The crisis deepens
June, 2017
An average of 4 people died from illicit drug use every day this May reports the BC Coroners Service.
A total of 129 British Columbians died of overdose in May 2017 – that’s a 158% increase over May 2016. Until November 2016, B.C. had never seen as many as 100 drug deaths in a single month. In every month since then, the number has exceeded 110, with the all-time high being December 2016 with 159 deaths.
The total overdose death toll for 2017 is now 640 people. That’s nearly twice the number at this time last year. 2016 is currently the deadliest year on record for overdoses in BC but it looks like 2017 will be even deadlier and officials are expecting over 1200 deaths with 7 more months before year’s end.
“The number of deaths shows that the risks remain extreme,” said Chief Coroner Lisa Lapointe, in a statement. “The drug supply is unsafe, and casual and occasional users are at high risk of overdose due to their opioid naiveté.”
The BC Coroners Service says that the proportion of illicit drug deaths where fentanyl was detected continues to climb. During 2016, the proportion of fentanyl-related deaths stayed the same at about 60% but in the first four months of 2017, that figure rose to 72%, indicating continued toxicity within the drug supply.
Heroin Assisted Treatment information
March, 2017
Visit our new page on Harm Reduction to learn about Harm Reduction, Heroin Assisted Treatment and more. For a powerful introduction, click on the link to learn from patients and staff at Vancouver’s Crosstown Clinic
Position Statement for the Support of Nurses Living with HIV
November, 2015
Read CANAC’s new Position Statement, here.
HIV core competencies
June, 2015
CANAC publishes the result of a pilot project on HIV core competencies.
Other Information
-
Get in Touch
If you need to contact a specific member, please visit our directory.
-
Mission Statment
The mission of CANAC is to recognize and foster excellence in HIV/AIDS nursing through education, mentorship and support. Read full statement.
-
Member Portal
Maintain your CANAC membership through our online
member portal.